Environmental exposures and pulmonary function among adult residents of rural Appalachian Kentucky
Estimated residential exposures of adults to roadway density and several metrics of resource extraction, including coal mining and oil and gas drilling, were hypothesized to contribute to the prevalence of respiratory disease in rural Appalachia.
Objective
Determine how small-area geographic variation in residential environmental exposures impacts measures of pulmonary function among adults in a community-based study.
Methods
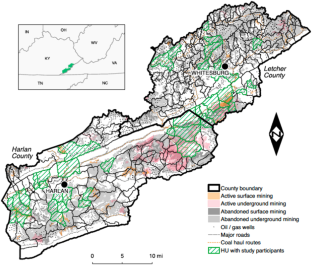
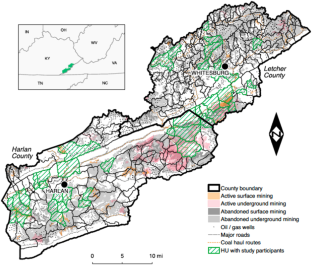
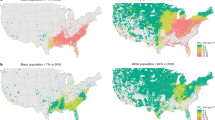
We examined associations between residential environmental respiratory exposures and pulmonary function among 827 adult participants of the “The Mountain Air Project”, a community-based, cross-sectional study in Southeastern Kentucky during 2016–2018. Exposures characterized the density of roadways, oil/gas wells, or current/past surface and underground coal mining at the level of 14-digit hydrologic unit code (HUC), or valley “hollow” where participants resided. Each participant completed an in-person interview to obtain extensive background data on risk factors, health history, and occupational and environmental exposures, as well as a spirometry test administered by experienced study staff at their place of residence. Multivariable linear regression was used to model the adjusted association between each environmental exposure and percent predicted forced expiratory volume in one second (FEV1PP) and forced vital capacity (FVCPP).
Results
Adjusted regression models indicate persons living in HUCs with the highest level of roadway density experienced a reduction in both FEV1PP (−4.3: 95% CI: −7.44 −1.15;) and FVCPP (−3.8: 95% CI: −6.38, −1.21) versus persons in HUCs with the lowest roadway density. No associations were detected between the metrics associated with mining and oil and gas operations and individual pulmonary function.
Impact statement
- Our work demonstrates the potential adverse impact of roadway-related exposures on the respiratory health of rural Appalachia residents. We employed a novel method of small-area exposure classification based on the hydrologic unit code (HUC), representing potential exposure levels per hollow occurring in proximity to the residence, and controlled for individual-level risk factors for reduced respiratory health. We highlight an overlooked yet ubiquitous source of residential exposure from motor vehicles that may contribute to the regionally high prevalence of respiratory disease in rural Appalachia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
265,23 € per year
only 44,21 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Air pollution exposure disparities in US public housing developments
Article Open access 14 June 2022

Exploring the adverse effect of fine particulate matter (PM2.5) on wildland firefighters’ pulmonary function and DNA damage
Article Open access 04 April 2024
Air pollution exposure disparities across US population and income groups
Article 12 January 2022
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
References
- Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Shirude S, Naghavi M, et al. Trends and patterns of differences in chronic respiratory disease mortality among US counties, 1980–2014. JAMA. 2017;318:1136–49. ArticlePubMedPubMed CentralGoogle Scholar
- Hendryx M. Personal and family health in rural areas of Kentucky with and without mountaintop coal mining. J Rural Health. 2013;29:s79–88. ArticlePubMedGoogle Scholar
- Hendryx M, Luo J. An examination of the effects of mountaintop removal coal mining on respiratory symptoms and COPD using propensity scores. Int J Environ Health Res. 2015;25:265–76. ArticlePubMedGoogle Scholar
- Kurth L, Kolker A, Engle M, Geboy N, Hendryx M, Orem M, et al. Atmospheric particulate matter in proximity to mountaintop coal mines: sources and potential environmental and human health impacts. Environ Geochem Health. 2015;37:529–44. ArticleCASPubMedGoogle Scholar
- Aneja AP, Pillai PR, Isherwood A, Morgan P, Aneja SP. Particulate matter pollution in the coal-producing regions of the Appalachian Mountains: Integrated ground-based measurements and satellite analysis. J Air Waste Manag Assoc. 2017;67:421–30. ArticleCASPubMedGoogle Scholar
- Macey GP, Breech R, Chernaik M, Cox C, Larson D, Thoma D, et al. Air concentrations of volatile compounds near oil and gas production: a community-based exploratory study. Environ Health. 2014;13:82. ArticlePubMedPubMed CentralGoogle Scholar
- Boyles AL, Blain RB, Rochester JR, Avanasi R, Goldhaber SB, McComb S, et al. Systematic review of community health impacts of mountaintop removal mining. Environ Int. 2017;107:163–72. ArticleCASPubMedPubMed CentralGoogle Scholar
- Shaw T, DeYoung A, Rademacher EW. Educational attainment in Appalachia: growing with the nation, but challenges remain. J Appalach Stud. 2004;10:307–29. Google Scholar
- Michimi A, Wimberly MC. Spatial patterns of obesity and associated risk factors in the conterminous U.S. Am J Prev Med. 2010;39:e1–12. ArticlePubMedGoogle Scholar
- Mills CW, Johnson G, Huang TTK, Balk D, Wyka K. Use of small-area estimates to describe county-level geographic variation in prevalence of extreme obesity among US adults. JAMA Netw Open. 2020;3:e204–89. ArticleGoogle Scholar
- Cardarelli K, Westneat S, Dunfee M, May B, Schoenberg N, Browning S, et al. Persistent disparities in smoking among rural Appalachians: evidence from the Mountain Air Project. BMC Public Health. 2021;21:270–21. ArticlePubMedPubMed CentralGoogle Scholar
- Zhang KM, Wexler AS. Evolution of particle number distribution near roadways. Part I: analysis of dynamics and its implications for engine emission measurement. Atmos Environ. 2004;38:6643–53. ArticleCASGoogle Scholar
- Morawska L, Ristovski Z, Jayaratne R, Keogh D, Ling X. Ambient nano and ultrafine particles from motor vehicle emissions: characteristics, ambient processing and implications on human exposure. Atmos Environ. 2008;42:8113–38. ArticleCASGoogle Scholar
- Heinrich J, Topp R, Gehring U, Thefeld W. Traffic at residential address, respiratory health, and atopy in adults: the National German Health Survey 1998. Environ Res. 2005;98:240–9. ArticleCASPubMedGoogle Scholar
- Kan H, Heiss G, Rose KM, Whitsel E, Lurmann F, London S, et al. Traffic exposure and lung function in adults: the Atherosclerosis Risk in Communities study. Thorax. 2007;62:873–9. ArticlePubMedPubMed CentralGoogle Scholar
- Balmes JR, Earnest G, Katz PP, Yelin EH, Eisner MD, Chen H, et al. Exposure to traffic: lung function and health status in adults with asthma. J Allergy Clin Immunol. 2009;123:626–31. ArticlePubMedPubMed CentralGoogle Scholar
- Rice MB, Ljungman PL, Wilker EH, Dorans KS, Gold DR, Schwartz J, et al. Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am J Respir Crit Care Med. 2015;191:656–64. ArticleCASPubMedPubMed CentralGoogle Scholar
- Rice MB, Rifas-Shiman SL, Litonjuan AA, Oken E, Gillman MW, Kloog I, et al. Lifetime exposure to ambient pollution and lung function in children. Am J Respir Crit Care Med. 2016;193:881–8. ArticleCASPubMedPubMed CentralGoogle Scholar
- Carlsen HK, Modig L, Levinsson A, Jeong-Lim K, Toren K, Nyberg F, et al. Exposure to traffic and lung function in adults: a general population cohort study. BMJ Open. 2015;5:e007624. ArticlePubMedPubMed CentralGoogle Scholar
- Penttinen P, Timonen KL, Tiittanen P, Mirme A, Ruuskanen J, Pekkanen J. Number concentration and size of particles in urban air: effects on spirometric lung function in adult asthmatic subjects. Environ Health Perspect. 2001;109:319–23. ArticleCASPubMedPubMed CentralGoogle Scholar
- McCreanor J, Cullinan P, Nieuwenhuijsen M, Stewart-Evans J, Malliarou E, Jarup L, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N. Engl J Med. 2007;357:2348–58. ArticleCASPubMedGoogle Scholar
- Lipfert F, Wyzga R. On exposure and response relationships for health effects associated with exposure to vehicular traffic. J Expo Sci Environ Epidemiol. 2008;18:588–99. ArticleCASPubMedGoogle Scholar
- ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute. 2011.
- May BA, Cardarelli KM, Silver R, Christian WJ, Schoenberg NE, Browning SR. Hollows as sampling units for community-based participatory research in Appalachia: the mountain air project. Prog Community Health Partnerships: Res, Educ, Action. 2019;13:401–10. ArticleGoogle Scholar
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87. ArticleCASPubMedGoogle Scholar
- R Development Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing 2011. http://www.r-project.org (accessed March 9, 2022).
- Venn A, Yemaneberhan H, Lewis S, Parry E, Britton J. Proximity of the home to roads and the risk of wheeze in an Ethiopian population. Occup Environ Med. 2005;62:376–80. ArticleCASPubMedPubMed CentralGoogle Scholar
- Hart JE, Eisen EA, Laden F. Occupational diesel exhaust exposure as a risk factor for chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2012;18:151–4. ArticleCASPubMedPubMed CentralGoogle Scholar
- Nitschke M, Appleton SL, Li Q, Tucker GR, Shah P, Bi P, et al. Lung function reductions associated with motor vehicle density in chronic obstructive pulmonary disease: a cross-sectional study. Respir Res. 2016;17:138. ArticlePubMedPubMed CentralGoogle Scholar
- Christian WJ, Flunker J, May B, Westneat S, Sanderson WT, Schoenberg N, et al. Adult asthma associated with roadway density and housing in rural Appalachia: the Mountain Air Project (MAP). Environ Health. 2023;22:28. ArticlePubMedPubMed CentralGoogle Scholar
- Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu Rev Public Health. 2002;23:303–31. ArticlePubMedGoogle Scholar
- Li W, Dorans KS, Wilker EH, Rice MB, Schwartz J, Coull BA, et al. Residential proximity to major roadways, fine particulate matter, and adiposity: the Framingham heart study. Obesity. 2016;24:2593–9. ArticlePubMedGoogle Scholar
Acknowledgements
We gratefully acknowledge the leadership and contributions of Nancy Schoenberg, PhD, as a co-investigator of the study, Beverly May, DrPH, and Nell Fields of the Mountain Air Project staff, and the contributions of the Mountain Air Project Community Advisory Board. Susan Westneat, MA, provided data management and statistical and analytic support on the study. We recognize the editorial and technical support of Steve Claas of the Office of Scientific Writing at the University of Kentucky. We also acknowledge the tireless efforts of the community health workers including Darlene Warf, Betty Keith, Denise Baird, Libby Honeycutt, and Penny Lee who recruited participants and administered surveys and spirometry tests. Finally, we acknowledge the time and efforts of the participants in the Mountain Air Project and are grateful for their participation.
Funding
The authors received support for this work from three federal grants: NIEHS R01 ES024771; NIEHS P30 ES026529; and CDC/NIOSH T42 OH010278 This work was supported by NIEHS R01ES024771-01, CDC/NIOSH T42OH010278, and NIH/NIEHS T32ES015459.
Author information
Authors and Affiliations
- Department of Environmental and Occupational Health Sciences, University of Washington School of Public Health, Seattle, WA, USA John C. Flunker
- Department of Biosystems and Agricultural Engineering, College of Agriculture, Food, and the Environment, University of Kentucky, Lexington, KY, USA Wayne T. Sanderson
- Department of Epidemiology, College of Public Health, University of Kentucky, Lexington, KY, USA W. Jay Christian & Steven R. Browning
- Department of Pulmonology, College of Medicine, University of Kentucky, Lexington, KY, USA David M. Mannino
- John C. Flunker